by charmnicole | May 3, 2018 | Blog, Tips to Help, Updates

June 2016 we served our 100th family. Since then we’ve passed milestones of service such as 1000 families served and 100 families served in a month.
Currently, we provide services for ten families on an average day. About 300 families per month.
We anticipate with the launch of our Free Spotlight Hope APP that we will soon be able to reach and serve nearly all of the families impacted by Pediatric Cancer.
That’s about 17,000 families per year, just for the new cases.
To grow to this level of service we need your help.
We are all volunteer, and 100% of contributions go toward our Program Services. We currently serve the families we work with at the tremendously efficient rate of just $20 per family.
If you think it’s worth supporting a family who can benefit from our programs, please become a BraveHeart today, and sponsor at the level that is right for you.
Perhaps you could sponsor a family? ($20)
Perhaps you could sponsor a day? ($200)
Or a week? ($1400) of current service.
Please go to: https://braveheartsforkids.org/donation-form/ and do whatever you can.
Become a BraveHeart today.

And Thank You! Your support means everything to our BraveHearts Kids and their families!

by admin | Dec 2, 2016 | Blog, Latest Pediatric Cancer News, Updates
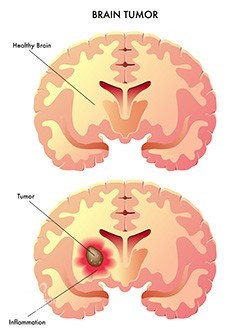
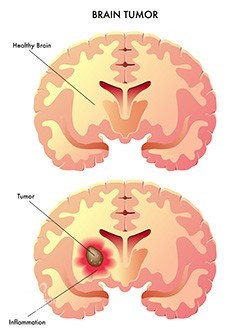
Children that are diagnosed with the severe brain tumour malignant glioma often have a very poor prognosis, partly due to the fact that knowledge about how paediatric malignant gliomas occur and develop is very limited.
According to a new research study, Mouse Models of Paediatric Supratentorial High-Grade Glioma Reveal How Cell of Origin Influences Tumour Development and Phenotype, conducted at Uppsala University and published in the journal Cancer Research, glioma development and glioma cell properties in mice are affected by both age and the cell type from which the tumour has arisen. The tumour cell of origin was also important for the susceptibility of the tumour cells towards cancer drugs.
The brain is composed mainly of two types of cells; neurons and supportive cells called glial cells. Gliomas are brain tumours that are similar to glial cells. Malignant glioma is the most common form of primary brain tumour in adults; it is relatively rare in children, but the prognosis for both adults and children is very poor. Of all childhood cancers, malignant glioma is among the most lethal.
Due to the fact that there have not been that many studies of malignant glioma in children, more knowledge and relevant disease models are necessary to improve the possibilities to find efficient drugs.
Most studies in the field of childhood malignant glioma have to date focused on the genetics of the disease; there is therefore a dire lack of knowledge about in which cell type the tumour originates and how this particular cell type affects the properties of the tumour.
The researchers in this latest study used mouse models of glioma and found that malignant glioma originating from different cell types behave differently. They induced glioma tumours from both undifferentiated stem cells, that can give rise to both neurons and glial cells, and from oligodendrocyte precursor cells (OPC), that are more differentiated and can only give rise to glial cells.
‘It turned out that tumours originating from stem cells were both more frequent and more aggressive as compared to those that originated from OPC. A very interesting finding was that tumour cells that had originated from undifferentiated stem cells were more susceptible to a range of cancer drugs,‘ says Lene Uhrbom who has led the study at the Department of Immunology, Genetics and Pathology.
The researchers also compared how the tumours developed in young mice as compared to adult mice and found that both age and cell of origin are important for tumour development. Furthermore, they could show that their tumour models in young mice were highly similar to a subgroup of malignant glioma in children.
‘We have developed new models that are relevant for studies of childhood malignant glioma. There is a lack of such models and we believe that these can become very useful in further studies to uncover the underpinnings of this devastating disease.
Our finding that the cell of origin could influence the response to treatment also shows that is important to identify clinically relevant subgroups of childhood malignant glioma, to be able to design the most efficient therapy for each patient. Our next challenge will be to find out how different cells of origin for glioma gives rise to these differences and to identify new targets for therapy,‘ says Lene Uhrbom.
Source: Little Fighters Cancer Trust | Author: LFCT




Most Commented