Causes, Risk Factors, and Prevention of Childhood Brain and Spinal Cord Tumors
What causes brain and spinal cord tumors in children?
Generally speaking, “cancer” is a broad name for a condition in which cells in a particular part of the body begin to malfunction. They begin to grow, divide, and replicate more quickly than normal cells, and/or they do not die as normal when they are worn out or damaged. When these abnormal, or “cancerous”, cells originate in the brain or the spinal cord, they usually form a clump or a mass known as a tumor. As the cancerous cells continue to replicate, the tumor grows until it begins to cause damage to the brain and/or the spinal cord.
Scientists are still trying to learn exactly why some cells grow, function, and die normally, while others grow abnormally and develop into a brain or spinal cord tumor. Brain and spinal cord tumors are most likely caused by mutations (random changes) in the DNA within each cell (our DNA provides instructions governing the function of each cell in our body, and ultimately how our body looks and functions as a whole). Specifically, scientists believe that mutations to two specific types of genes may be the ultimate cause of brain and spinal cord tumors in children: oncogenes control when cells grow and divide and tumor suppressor genes slow down cell division and instruct cells to die at the proper time. Whether inherited from parents or spontaneous and random, mutations to these particular genes may cause cells to malfunction and ultimately become cancerous.
Ultimately, however, scientists do not know why these mutations occur, especially in children. While lifestyle choices such as smoking can cause genetic mutations (and thus cancer) in adults, there are no known lifestyle risks associated with childhood brain and spinal cord tumors in children. Unfortunately, the genetic mutations at the root of the tumor growth are simply random changes that cannot be predicted or prevented.
Are there risk factors for brain and spinal cord tumors in children?
A “risk factor” is anything that increases an individual’s chances of developing a disease like a brain or spinal cord tumor. As noted above, most cases of brain and spinal cord tumors in children appear to be caused by random genetic mutations without a known cause. There are very few known risk factors associated with this type of childhood cancer. The only two well-established risk factors are radiation exposure and certain rare inherited genetic conditions.
- Radiation exposure: exposure to large amounts of radiation is known to cause some types of cancer, including brain and spinal cord tumors in children. Now that this danger is known, the medical community takes active steps to avoid exposing the brain and central nervous system of children to radiation unless absolutely necessary. In some cases, radiation may be required as part of treatment for another type of cancer; in these cases, the benefits of treating one type of cancer must be weighed against the potential risk of developing a brain or spinal cord tumor in the future.
- Inherited genetic conditions: in less than 5% of cases of childhood brain and spinal cord tumors, children have an inherited genetic condition that may increase their risk of developing a tumor. These genetic syndromes themselves are exceedingly rare, and may include:
- Neurofibromatosis type 1 (von Recklinghausen disease)
- Neurofibromatosis type 2
- Tuberous sclerosis
- Von Hippel-Lindau disease
- Li-Fraumeni syndrome
- Gorlin syndrome (basal cell nevus syndrome)
- Turcot syndrome
- Cowden syndrome
- Hereditary retinoblastoma
- Rubinstein-Taybi syndrome
Can the development of brain and spinal cord tumors in children be prevented?
Can the development of brain and/or spinal cord tumors in children be prevented? This is a question many parents will ask themselves upon receiving the terrible diagnosis that their child has a brain or spinal cord tumor. The answer is always “no”. There is no known way to prevent or protect against brain or spinal cord tumors, and absolutely nothing that parents or guardians could have done to prevent this disease.
Source: Causes, Risk Factors, and Prevention of Childhood Brain and Spinal Cord Tumors








 Just because a food is white, doesn’t mean that it isn’t nutritious. In fact, white foods such as low-fat (1%) or fat-free milk, yogurt, and some cheeses are packed with vitamin D, calcium, and phosphorus.
Just because a food is white, doesn’t mean that it isn’t nutritious. In fact, white foods such as low-fat (1%) or fat-free milk, yogurt, and some cheeses are packed with vitamin D, calcium, and phosphorus. The natural plant pigment chlorophyll colours green fruits and vegetables. In our system, the green foods represented those foods rich in isothiocyanates, which induce enzymes in the liver that assist the body in removing potentially carcinogenic compounds.
The natural plant pigment chlorophyll colours green fruits and vegetables. In our system, the green foods represented those foods rich in isothiocyanates, which induce enzymes in the liver that assist the body in removing potentially carcinogenic compounds. A variation of the green colour category, these foods exhibit a richness in lutein, which is particularly beneficial for eye health. They also contain a high amount of vitamin C.
A variation of the green colour category, these foods exhibit a richness in lutein, which is particularly beneficial for eye health. They also contain a high amount of vitamin C. Orange foods are rich in beta-carotene, which are particularly good antioxidants. They are good for the heart, protect our eyes and also boost our immune system.
Orange foods are rich in beta-carotene, which are particularly good antioxidants. They are good for the heart, protect our eyes and also boost our immune system. Lycopene is the predominant pigment in reddish fruits and veggies. A carotenoid, lycopene is a powerful antioxidant that has been associated with a reduced risk of some cancers, especially prostate cancer, and protection against heart attacks.
Lycopene is the predominant pigment in reddish fruits and veggies. A carotenoid, lycopene is a powerful antioxidant that has been associated with a reduced risk of some cancers, especially prostate cancer, and protection against heart attacks. The blue/purple hues in foods are due primarily to their anthocyanin content; the darker the blue hue, the higher the phytochemical concentration. Blueberries are considered to have the highest antioxidant activity of all foods.
The blue/purple hues in foods are due primarily to their anthocyanin content; the darker the blue hue, the higher the phytochemical concentration. Blueberries are considered to have the highest antioxidant activity of all foods.
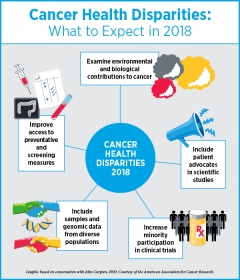
 Up until now, drug companies have been free to decide whether to pursue treatments for paediatric cancers as part of their work on adult cancers or not, and this has led to a minimal amount of new drugs specifically for paediatric cancers being developed.
Up until now, drug companies have been free to decide whether to pursue treatments for paediatric cancers as part of their work on adult cancers or not, and this has led to a minimal amount of new drugs specifically for paediatric cancers being developed. said Jorge Luis Lopez, a Miami attorney who sits on the board of the American Cancer Society. “We urge Donald Trump to sign this legislation into law and unleash American innovation and creativity for the health and well-being of all our children.”
said Jorge Luis Lopez, a Miami attorney who sits on the board of the American Cancer Society. “We urge Donald Trump to sign this legislation into law and unleash American innovation and creativity for the health and well-being of all our children.”
Most Commented